Introduction
Unhealthy lifestyles, including excessive alcohol consumption, smoking, poor diet, and sedentary habits, have significantly contributed to the global rise in cardiovascular disease. These factors often lead to obesity and diabetes, further exacerbating cardiovascular risk. While genetic factors may play a role, lifestyle choices remain a primary driver.
To prevent and manage cardiovascular diseases, it is crucial to mitigate risk factors such as high cholesterol, high blood pressure, diabetes, obesity, and excessive alcohol or tobacco use. A holistic approach encompassing diet, exercise, stress reduction, and medical intervention is essential for maintaining good cardiovascular health. By addressing these factors, individuals can significantly reduce their risk of heart attacks, strokes, heart failure, and atherosclerosis.
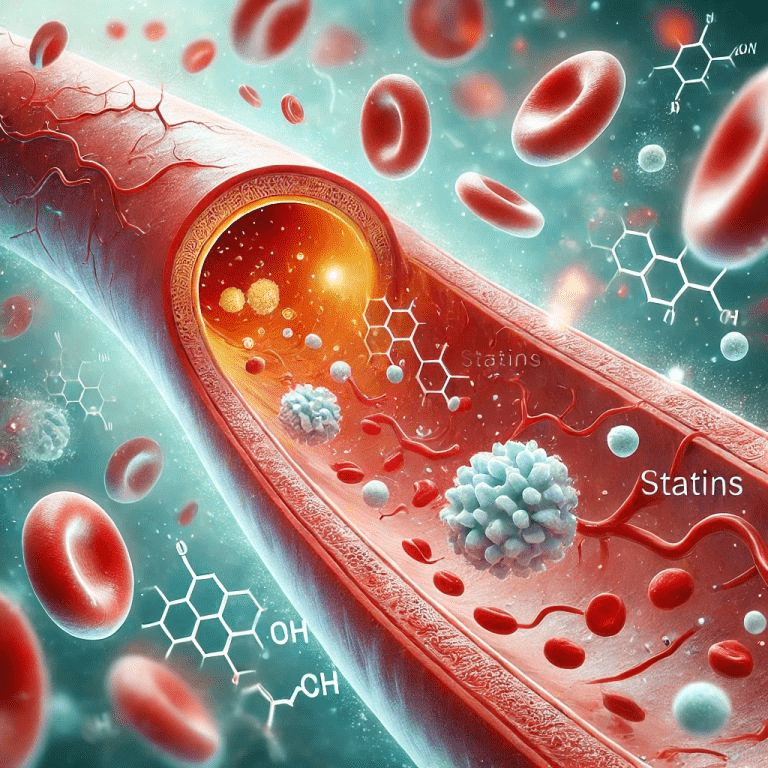
The Role of Statins in Managing Cardiovascular Risks
Statins are primarily used to lower LDL (“bad”) cholesterol levels in the blood, which may cause plaque buildup in arteries (atherosclerosis), leading to heart attacks and strokes. Statins are often prescribed to individuals with high LDL cholesterol levels, diabetes, hypertension, or those who are at an increased risk of cardiovascular diseases.
Statins have been shown to effectively lower not only LDL cholesterol but also VLDL and triglyceride levels. Clinical studies have demonstrated that statins can reduce LDL cholesterol by 20-60% and triglycerides by 10-30% in individuals with elevated levels.
While statins have a more significant impact on LDL cholesterol, their effect on VLDL is less pronounced and more variable. This is likely due to the close relationship between VLDL and triglycerides, with VLDL acting as a carrier for triglycerides in the bloodstream. The reduction in VLDL levels is often a secondary effect of statin therapy, resulting from the long-term improvement in lipid metabolism.
While statins don’t treat cardiovascular diseases directly, they play a preventive role, especially in people with existing heart conditions or at high risk for such diseases.
The Working of Statins
Statins are a class of medications known as 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors. Their primary course of action involves inhibiting the enzyme HMG-CoA reductase, which is responsible for the production of cholesterol in the liver. Statins also improve endothelial (the lining inside arteries) function, reduce inflammation, and stabilize atherosclerotic plaques. Through these mechanisms of action, statins effectively lower LDL cholesterol levels, reducing the risk of cardiovascular diseases.
Effectiveness of Statins
Statins are prescribed after monitoring lipid levels (lipid profile tests) to control LDL cholesterol. The dosage and duration of therapy are decided based on individual profiles, histories, risk factors, and long-term treatment plans.
Several studies, clinical trials, and research findings prove the effectiveness of statins in reducing cardiovascular risks.
- Law (2003) conducted randomized, placebo-controlled trials to assess the effectiveness of various statins in lowering LDL cholesterol levels and the impact of this cholesterol-lowering effect on reducing the risk of ischemic heart disease (IHD) events and stroke. The study concluded that statins can lower LDL cholesterol levels by an average of 1.8 mmol/l, leading to a significant reduction in the risk of IHD events by about 60% and stroke by 17%.
- A 2006 study by Kurian et al. explored the potential of statins beyond cholesterol reduction. They found that statins can stabilize atherosclerotic plaques, reduce inflammation, improve endothelial function, and even exhibit mild antihypertensive effects. These additional benefits, coupled with their cholesterol-lowering properties, make statins a valuable tool in preventing heart failure and other cardiovascular diseases.
- Kearney et al. (2008) conducted a meta-analysis consisting of randomized trials of statins to evaluate the efficacy of statin therapy on cholesterol-lowering in people with diabetes. It was found that statin therapy caused reductions in cardiovascular-related mortalities, major cardiovascular events, myocardial infarction, coronary revascularization, and stroke in people with diabetes.
When to Start a Statin Therapy
An individual is subjected to a statin therapy by a medical professional following one or more course of events:
- Identification of cardiovascular risk factors such as high blood pressure, diabetes, obesity, excessive alcohol consumption, smoking, or family history of heart disease.
- Noticing high blood cholesterol levels during a routine blood test, including a lipid profile, that measures cholesterol levels.
- A diagnosis of high cholesterol levels conducted following cardiovascular disease symptoms such as chest pain or discomfort, shortness of breath, especially during exertion or stress, fatigue, pain or discomfort in other areas such as arms, back, neck, jaw, or stomach, excessive and abnormal sweating, nausea, or palpitations.
If symptoms are minor, an initial treatment plan may include lifestyle modifications and regular monitoring of blood cholesterol. However, when the clinical diagnosis tests confirm high levels of cholesterol or other risk factors, the individual may be immediately subjected to statin therapy. Often, medication is supported by lifestyle changes, regular monitoring of cholesterol levels and other factors, and adjusting dosage and timing based on current lipid profile and existing conditions.
Factors Influencing the Effectiveness of Statins
The effectiveness of statins depends on several factors, including dosage, the timing of administration, patient compliance, and individual health profiles.
Dosage
High statin doses control higher LDL cholesterol levels since they effectively inhibit the HMG-CoA reductase enzyme, lowering cholesterol synthesis. Studies have shown that high-intensity statin therapy achieved through high statin doses reduces cardiovascular risks. However, higher doses carry the risks of higher side effects such as muscle pain and liver damage. Hence, the optimal statin dose is determined by individual risk factors such as sex, cholesterol levels, and existing cardiovascular health conditions.
Timing of administration
The body naturally produces cholesterol, with peak production occurring at night. This rhythm is influenced by factors like circadian rhythm, hormones, and metabolic needs influence this rhythm.
Short-acting statins, with a half-life of 1-3 hours, are metabolized quickly. To optimize their effectiveness, they are often administered in the evening when cholesterol production is highest.
Long-acting statins, with a half-life of 14-19 hours, are metabolized more slowly. This allows for less frequent dosing, often once daily, regardless of the time of day.
However, individual factors and specific medication formulations may influence the optimal timing of statin administration.
Patient compliance
Adhering strictly to the prescribed dosage, timing, and duration of statin therapy is crucial for its effectiveness. Non-compliance can diminish the drug’s potency, leading to elevated cholesterol levels and increased cardiovascular risk.
To ensure optimal outcomes, ongoing support from healthcare professionals and family members and regular medical follow-ups are essential. Patient education, addressing side effects, and simplifying treatment regimens, such as prescribing long-acting statins or combination therapies, can further enhance adherence.
Individual health profiles
Healthcare professionals actively consider individual health profiles while prescribing statin therapies due to their influence on the medication’s efficiency. The most important factors include age, genetics, gender, liver function, and existing conditions such as diabetes or kidney disease. These factors can affect the metabolism and absorption of statins, and adjustments in statin type, dosage, timing, and duration ensure maximum efficacy.
For example, individuals with liver impairments might need dose adjustments to rule out side effects. Genetic evaluations might be required to identify the most suitable statin type that ensures maximum efficacy on the detected enzyme variation. Hence, formulating personalized statin therapies based on health profiles ensures the best outcomes with minimal risks.
Risks and Benefits of Statin Therapy
While statins are highly effective in managing cardiovascular health, like any medication, they can have potential side effects, particularly with long-term use. Healthcare professionals carefully weigh these risks against the benefits when prescribing statin therapy.
To minimize risks and maximize efficacy, regular monitoring of lipid profiles and overall health is crucial. This allows for timely adjustments to medication, dosage, or treatment plans as needed. Additionally, considering individual health profiles and addressing any underlying conditions can further optimize the benefits of statin therapy.
Benefits of Statin Therapy
Statins are primarily prescribed to lower LDL cholesterol, a key factor in reducing the risk of heart disease and stroke. Beyond this primary function, statins offer additional cardiovascular benefits such as stabilizing plaque buildup in arteries, reducing inflammation, and improving blood vessel function. Emerging research, like the study by Young-Xu et al. (2003), suggests potential cognitive benefits, particularly with long-term use. Additionally, studies like Geifman et al. (2017) have shown potential reductions in cognitive decline among elderly patients on statin therapy.
Potential Side Effects of Statin Therapy
Statins are generally well tolerated by most individuals, even though some may encounter side effects. Muscle pain has been reported as the most common side effect. Digestive issues like indigestion, constipation, or diarrhea, as well as headache, have been reported in some individuals.
The less common side effects often associated with long-term statin therapy are liver damage, mild cognitive issues, or peripheral neuropathy. Some studies suggest that statins may slightly increase blood sugar levels, particularly in people with diabetes or prediabetes.
Regular check-ups with healthcare providers are essential to managing any risks and side effects and making remedial measures and adjustments to ensure the maximum efficacy of statin therapy.
Final Thoughts
Statins have been at the forefront of managing cardiovascular health, minimizing risk factors, and preventing cardiovascular diseases for several decades. Starting with the first statin, lovastatin, in 1987, this class of medications has effectively treated high cholesterol to prevent heart disease.
The success of any statin therapy is determined by diligent consideration of efficiency factors, regular monitoring of the lipid profile, and management of risk factors and side effects. Along with regular healthcare follow-ups, lifestyle modifications to support the therapy are essential for achieving maximum benefit and ensuring good cardiovascular health.
References
- Law, M. R. (2003). Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ, 326(7404), 1423–0. https://doi.org/10.1136/bmj.326.7404.1423
- Kurian, K. C., Rai, P., Sankaran, S., Jacob, B., Chiong, J., & Miller, A. B. (2006). The Effect of Statins in Heart Failure: Beyond its Cholesterol-Lowering Effect. Journal of Cardiac Failure, 12(6), 473-478. https://doi.org/10.1016/j.cardfail.2006.02.001
- Kearney, P. M., Blackwell, L., Collins, R., Keech, A., Simes, J., Peto, R., Armitage, J., & Baigent, C. (2008). Efficacy of cholesterol-lowering therapy in 18 686 people with diabetes in 14 randomised trials of statins: a meta-analysis. The Lancet, 371(9607), 117–125. https://doi.org/10.1016/s0140-6736(08)60104-x
- Young-Xu, Y., Chan, K., Liao, J. K., Ravid, S., & Blatt, C. M. (2003). Long-term statin use and psychological well-being. Journal of the American College of Cardiology, 42(4), 690–697. https://doi.org/10.1016/s0735-1097(03)00785-x
- Geifman, N., Brinton, R. D., Kennedy, R. E., Schneider, L. S., & Butte, A. J. (2017). Evidence for benefit of statins to modify cognitive decline and risk in Alzheimer’s disease. Alzheimer S Research & Therapy, 9(1). https://doi.org/10.1186/s13195-017-0237-y